S.Valentine Fernandez
The operation of rhinoplasty demands a thorough understanding of an art and science.Some complications of rhinoplasty relate to anesthesia and do not fall within the bounds of this discussion.
Complications of rhinoplasty may be divided into 4 basic categories as follows:
- Intraoperative
- Immediate post operative (in the recovery ward)
- Early postoperative
- Late postoperative
A practical approach to aesthetics in the nose begins with an accurate assessment. Frontal views define x-axis (width) and y-axis (height) deformities, lateral views define z-axis (depth/projection) and y-axis deformities, and basal views define x-axis and z-axis deformities. Based on these views, a 3-dimensional concept of the nose is made available for manipulation. The goal of rhinoplasty is to improve the existing harmony without causing functional impairment.
According to the literature, the complication rate for nasal surgery varies from 4-18.8%. In individual hands, this rate generally falls as surgical experience accumulates. Skin and associated soft tissue complications occur in up to 10% of cases. According to estimates, severe systemic or life-threatening complications occur in 1.7-5% of rhinoplasty cases. Intracranial complications are rare.
The clinical manifestation of rhinoplasty complications may broadly be classified as follows:
- Functional
- Infectious
- Aesthetic
- Psychological
- Specific to complication
Intraoperative complication:
1. Excessive bleeding 2. Tears of mucoperichondrial flaps 3. Buttonholing of skin 4. Cautery burns5. Collapse of bony pyramid:
- Collapse of the bony pyramid may occur during removal of a bony hump with an osteotome, particularly when the patient has had previous nasal trauma or if the vomer or ethmoid have been weakened as a result of previous surgery. Rasping may be advisable in these circumstances.
- Rectification requires careful approximation of the segments and provision of adequate internal and external splint support during healing.
7. Osteotomy complications
- "Rocker" deformity: This deformity results when the medial osteotomy creates a cephalic fracture higher in the thicker part of the frontonasal junction. Attempted narrowing after the osteotomies results in lateralization of the superior segment of the fractured bones, based on a fulcrum at or about the radix. Repositioning the cephalic fracture lower on the nasal bone rectifies this deformity.
- "Open roof" deformity: When the lateral segments fail to align with the septal dorsum following osteotomies, a gap, which may be visually and palpably obvious, results. If neglected, the intranasal mucous membrane adheres to the overlying soft tissue and may create a depression at the site. If alignment failure is unilateral, the nose appears asymmetric. Correction involves assuring centralization of the septum and complete medial mobilization of the lateral segments following osteotomy. Usual causes of open roof deformity include the following:
- Greenstick cephalic fracture during osteotomies (will return to its preoperative position)
- Failure to adequately mobilize the fractured segments medially
- Excessive nasal packing
- Uncorrected deviated perpendicular plate of the ethmoid (may prevent medialization of the lateral segments)
- "Step" deformity: This deformity may result if a single lateral osteotomy is performed too far medial to the nasofacial groove, with a visible ridge on the side of the nose. Correction involves repeating the osteotomy at the correct level.
Immediate post operative complications:
1. Airway obstruction 2 Anaphylaxis: This is a distinct possibility when intraoperative
antibiotic medication is used. Anaphylactic shock subsequent to
bacitracin nasal packing has been reported, and latex anaphylaxis is
well document 3. Visual impairmentEarly post operative complications:
1. Hemorrhage: Reported prevalence of hemorrhage varies from 2-4%. 2. Septal hematoma:
3. Infection: Wound infection, Septicemia, Toxic shock syndrome, subacute bacterial endocarditis, intracranial infections, and acute &/or chronic sinusitis.
4. Dehiscence of incisions: The transcolumellar incision must be attended to immediately, or a scar will form, contributing to a poor result.
5.Persistent edema: Persistent edema and numbness over the nasal tip region may occur following external rhinoplasty and may last several months. This is not a problem if the patient has been forewarned.
6. Skin necrosis: Excessive undermining, injudicious cautery use, and overzealous skin thinning may lead to skin necrosis. This may cause an impaired blood supply and infection. Similarly, a tight dressing may cause vascular impediment and skin necrosis. Debridement and secondary healing is encouraged if necrosis occurs. Later, local steroid injection, dermabrasion, laser modification, and/or flap reconstruction may be necessary to aid scar aesthetics. Skin necrosis may also result from dorsal augmentation, in which case removal of the augmenting material may be necessary.
7. Sequestra formation, 8. Cardiovascular insufficiency 9. Cerebrospinal fluid rhinorrhea 10. Contact dermatitis 11. Nasal blockage 12. Numbness and pain 13. Olfactory disturbance: Patients with past facial trauma may be predisposed to injury of the olfactory apparatus during osteotomy. 14. Carotid-cavernous fistula 15. Reassurance demand: A small number of patients need the surgeon to repeatedly express that the nasal blockage will disappear, the smell and taste sensation will return, the teeth anesthesia will subside, and the tip projection and swelling will decrease in time.Early psychological complications: Transient episodes of anxiety or depression are not uncommon and may last up to 6 weeks after the operation
Late postoperative complications
1. Scar hypertrophy: This may detract from a good result following an external rhinoplasty. Skin loss from infection and necrosis is a disaster. Aim initial attempts at reducing the size of the scar with intralesional steroids. Further treatment could include dermabrasion, lasers, and/or surgical scar revision.
2. Polly beak nasal deformity-This deformity is characterized by absence of the supratip dip (ptosis tip) may present in degree.
3. Synechiae formation 4. Septal perforation: The prevalence of this complication has been described as 3-24.5%.
5. Nasal valve collapse: Aggressive cephalic trim of the lower lateral cartilages may provoke this complication. Collapse may cause airway distress and is a source of patient discontent. Cartilage spreader grafts may prove useful for internal valve collapse. Alar batten grafts improve external valve collapse.
6. Nasal stenosis This is a disaster when it occurs, and it may be related to circumscribed incisions with excessive lining removal. Stenosis causes airway obstruction and is a source of persistent discomfort. Reconstructive surgery may provide some relief.
7. Bossa formation
- Bossae are protuberances that may arise in the region of the nasal tip. Their postoperative incidence is quoted at 2%.
- While bilateral symmetric occurrences may assume a pleasing appearance, bilateral asymmetric and unilateral bossae demand surgical attention. During operation, ensuring that the remnant lower lateral cartilages are of equal dimensions on both sides is important.
- Bossae usually occur in noses with preoperative asymmetry, use of destructive rhinoplasty techniques, thin skin, and excessive postoperative scarring. The triad of thin skin, strong cartilages, and bifidity also indicate the patient who is prone to the development of bossae. Tip graft movement may also contribute to bossa formation.
11. Aesthetic surgical misjudgments
- Undercorrection or overcorrection of a preexisting deformity leads to either persistence of the deformity or to introduction of a new one. A new deformity may introduce a functional deficit. Some of these deformities are illusory, and correction only follows after an accurate diagnosis is made. Ideally, revision rhinoplasty should not be performed until at least 12 months after the initial operation.
- These deformities may occur singly or in combination and may relate as an x-axis (width), y-axis (height), or z-axis (depth) deformity/deformities in the various segments.
Upper third deformities
Deep nasofrontal angle, Shallow nasofrontal angle, Upper third widening, Upper third convexity, Upper third overreduction:, & Upper third asymmetry.
Middle third deformities
Middle third widening:, Middle third convexity, Middle third saddling, & Middle third asymmetry
Lower third deformities
Lower third widening or flaring, Tip widening or boxy tip, Tip narrowing or pinched tip, Tip asymmetry, Tip projection deformities, Wide columella, Hanging columella or "columella show", "Hanging" or "veiled" alae , Alar notching, Nostril asymmetry, Retracted nasolabial angle, Protracted nasolabial angle, &
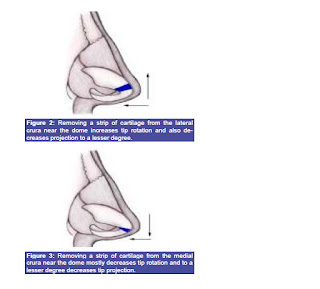
Alar collapse: Excessive removal of the lateral crura dampens support afforded by these structures, causing alar collapse and airway discordance. Reconstructive techniques with alar battens may be necessary in difficult cases.
Other
- Graft/implant migration: Migration may comprise resorption, displacement, or extrusion; it may be provoked by trauma and infection. Allografts have a higher extrusion and infection rate than autografts. An infected implant must be removed if antibiotics do not help. Revise displaced grafts causing aesthetic inconvenience with appropriate stabilization.
- The disproportionate nose: This nose does not fit the face and is not a credit to the surgeon's artistic skill. Reconstructive rhinoplasty techniques follow the patient's expression of discontent with original results.
- Underlying maxillofacial deformity: A superb rhinoplasty result may be ruined by the unmasking of a previously unnoticed or undiagnosed maxillofacial deformity. The maxillae and mandible with labial and dental components must be considered preoperatively and the patient must be forewarned. Attendance by a cosmetic dentist and inclusion of chin surgery may be necessary.
Persistent psychological complications: Several contradictory studies are available.
Thoracic and thoracolumbar instability, Gustatory rhinorrhea, Human adjuvant disease:, Lacrimal fistula, Enophthalmos and silent sinus syndrome.
For more detailed analysis see:
http://emedicine.medscape.com/article/843439-overview#showall
Some other complications not mentioned above: Neuropathic pain (temporary or permanent), Empty Nose Syndrome, Graft warping and resorption and complications from injectable material in the nose. For more info on this subjects check out my other blog posts. (See labels on right side column of my blog and click on any of the labels.)
See also:
http://www.youtube.com/watch?v=sj4RrAlAwXo
http://yourguidetoplasticsurgery.com/rhinoplasty-risks
http://www.emptynosesyndrome.org/what_is_ens.php
http://www.therhinoplastycenter.com/ComplicationsofRhinoplasty/complications1.html